Getting smart about hydrocephalus
We often take for granted that medical science marches on, ever more rapidly, with better understanding leading almost inevitably to better treatment. Yet when it comes to the common problem of hydrocephalus, well known to Hippocrates and other physicians of the ancient world, doctors are still using a method first developed in 1949 to relieve this potentially deadly condition.
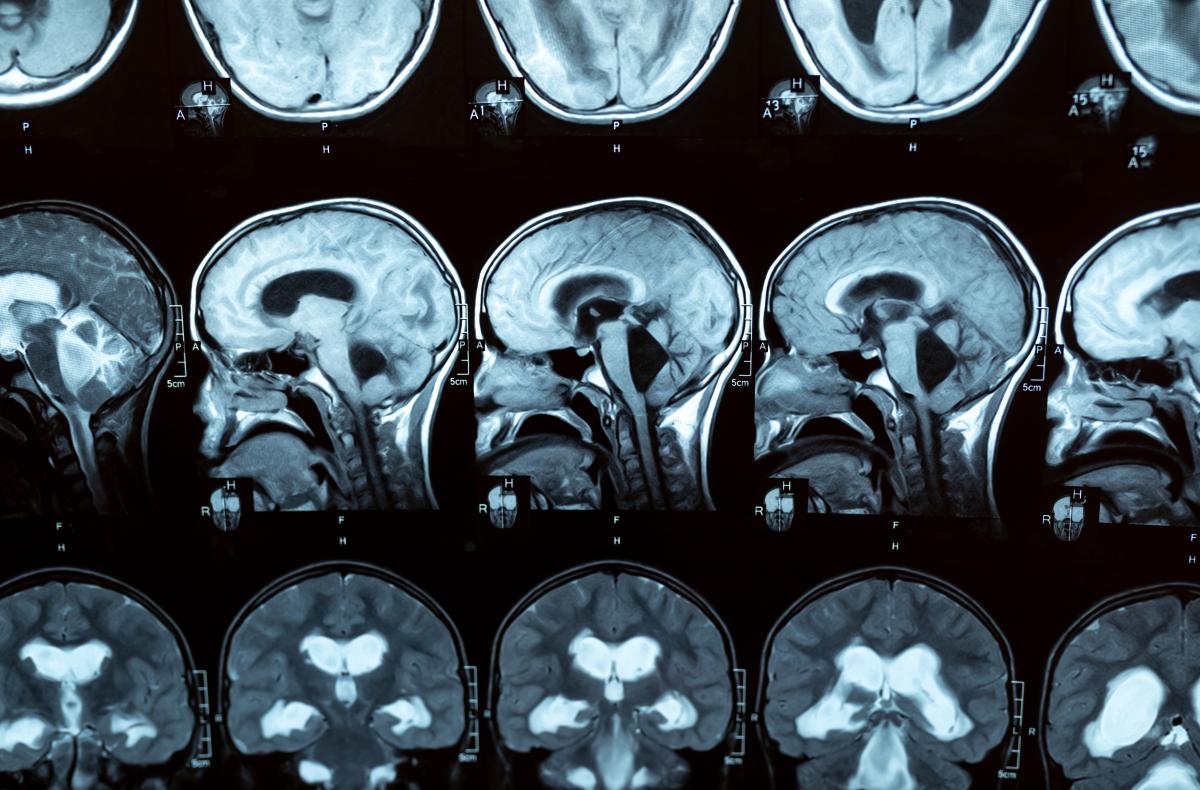
Hydrocephalus refers to a build-up of excess fluid in cavities in the brain (called ventricles), causing them to enlarge and possibly increase pressure on the brain. It’s far from uncommon around the world. In the US, around 1 in 500 babies are born with hydrocephalus, with more developing the condition in the first two years of life (the figures for Europe are not directly comparable but are available here). Nor is it restricted to children: in adults the condition can occur at any time, particularly after an intracranial infection or bleeding, or after the age of 60, with increasing prevalence with age. In fact, it is quite likely to be underdiagnosed in this age group, when symptoms may be ascribed to Alzheimer’s or Parkinson’s disease. Which of course means that many people – up to 10% of dementia patients – could be living with a treatable condition, not a degenerative one. Just think of what that could mean for quality of life, not only for the sufferers, but for their loved ones and carers.
The breakthrough that came 70 years ago
The consequences of untreated hydrocephalus range from brain damage to death, but fortunately, surgical treatment is very effective. Around a century ago, surgeons began developing shunts to drain the fluid away from the brain and into the abdominal cavity. Once valves were introduced (between 1949 and 1960), they became really useful, making it possible to drain the excess fluid automatically – either based on a preset pressure level, or adjustable by the clinician – and so greatly improving results.
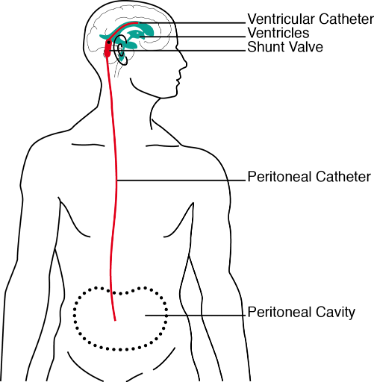
But there are still limitations. For instance, gravity may cause over-drainage when the patient is upright, and blockage or infections are common. Furthermore, the differential pressure valves based on the 70-year-old technology simply aren’t accurate enough to deliver good results consistently. Is it not time for an update?
Since starting her PhD in 2008, when she first talked to neurosurgeons about the problems of treating hydrocephalus, Dr Marianne Schmid Daners (with a background in both mechanical engineering and nursing) has been devoting herself to the challenge of designing a 21st-century shunt. A major handicap was the great lack of knowledge about the disease and the best parameters for controlling the shunt. After her PhD studies, Marianne followed a two-track approach, oriented to both basic research and application, with funding from the Swiss National Science Foundation and Innosuisse, respectively. All projects have been pursued in close collaboration with the University of Zurich, the University Hospital Zurich and international partners.
During the basic investigations, craniospinal, cardiovascular and abdominal pressures were measured in healthy adult sheep and quantified depending on posture changes and interventions, such as bolus injections or drug stimuli. From these results the interdisciplinary team concluded that to manage shunt drainage according to individual demand, the intracranial pressure, the flow through the shunt and the posture should be all taken into consideration, enabling the shunt to react to physiologic conditions.
The application-oriented project has focused on the development of a novel sensor, shunt design and control, as well as on an actuation system to introduce a hydrocephalus-like condition in sheep. Together with Fabian Flürenbrock and Professor Melanie Zeilinger, great strides were made with the focus project VIEshunt (VIE here standing for ventricular, intelligent and electromechanical shunt) – a revolutionary first attempt at automated control that earned Fabian the Young Investigators Award at the Hydrocephalus conference 2022. The VIEshunt even includes data communication capabilities to provide unprecedented insight into the internal workings of the shunt system and the patient’s health. This makes it possible to forestall malfunctions and complications, and can potentially be leveraged to provide customized individual therapy.
The VIEshunt formed the basis for the NCCR Automation follow-up project “Safe learning-based control of cerebrospinal fluid shunt with active valve”, pursuing the goal of investigating, among other things, how to monitor relevant vital signals and derive estimations of the current state of the disease; how to robustly control drainage of the cerebrospinal fluid (CSF), and adjust it to the patient’s needs; and how the physiological controller can safely learn from feedback in order to optimize and personalize shunt control.
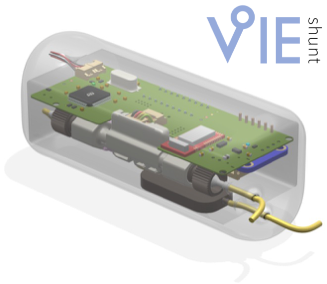
To achieve the desired leap forward, the project will leverage previous work in, on one side, the quantitative investigation into CSF dynamics, which delivers mathematical models to inform both design and testing, and on the other, the VIEshunt mechatronic system, which – with its sensors, actuators and embedded controllers – allows for the implementation and deployment of advanced control strategies that have not been attempted before.
The goal is not only to make CSF drainage safer and more physiological, but also to allow physicians and clinicians to gain a better understanding of the disease by enabling detailed long-term patient monitoring for the first time. This in turn should improve the design of future shunt systems and control algorithms, delivering sustained improvements in hydrocephalus therapy.
We still don’t know what causes this disease, and despite the tremendous impact it has on large numbers of sufferers, it has not attracted the attention given to problems like heart disease. We have learned a lot about it, though. Quantitative assessments, and intelligent shunts could help us learn even more – and will certainly contribute to much better patient care. That makes the novel automated shunt, emerging at the cutting edge of mechatronics and medical science, a particularly exciting contribution to global health and well-being.
Text written by Robynn Weldon and Marianne Schmid Daners.






